Latest news and views
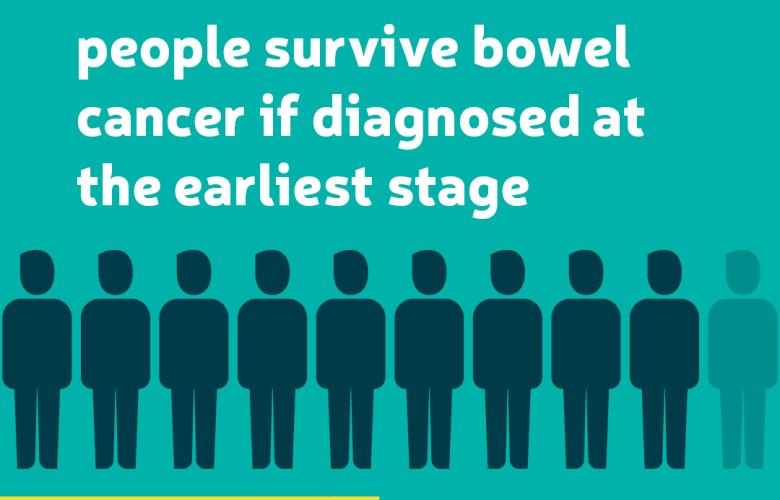
Bowel Cancer Awareness Month
April is Bowel Cancer Awareness Month, a fantastic annual opportunity to raise awareness of bowel cancer.
The earlier bowel cancer is spotted, the more treatable it’s likely to be. In fact, more than 9 in 10 people survive bowel cancer…
The earlier bowel cancer is spotted, the more treatable it’s likely to be. In fact, more than 9 in 10 people survive bowel cancer…
News
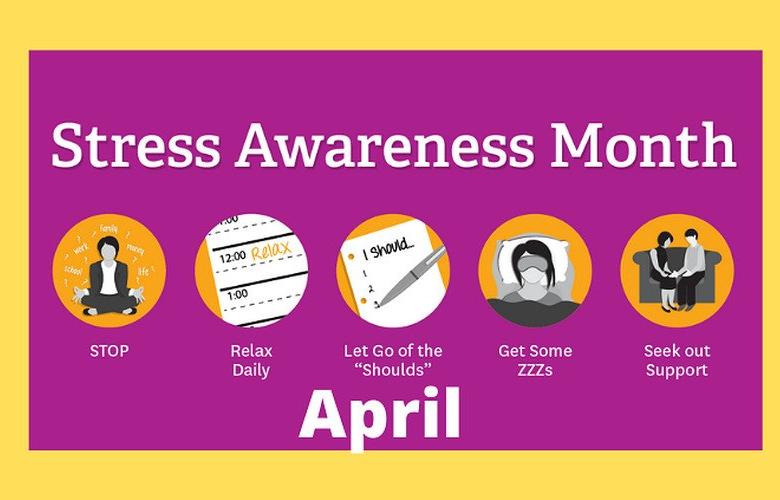
Stress Awareness Month 2024
The theme of this years Stress Awareness Month is #LittleByLittle and highlights the transformative impact of consistent, small positive actions on over-all wellbeing.
The Stress Management Society, explain how even the smallest steps taken each…
The Stress Management Society, explain how even the smallest steps taken each…
News

Deaf and hard of hearing people's healthcare experiences
It's important that deaf and hard-of-hearing people can get information in an accessible way. But feedback suggests not all services are complying with key legislation.
Blog
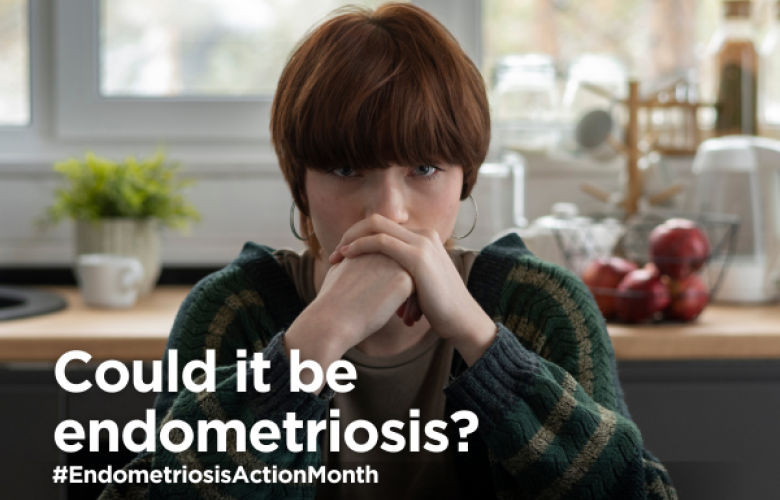
Years of being “dismissed, ignored and belittled”: Endometriosis UK urges improvement to deteriorating diagnosis times .
Getting a diagnosis for endometriosis now takes almost a year longer than before the pandemic, according to new research published by the charity Endometriosis UK during Endometriosis Action Month 2024 (March).
A new study shows that…
A new study shows that…
News

Share your feedback to improve care in your community
‘Share for Better Care’, a new campaign launched by Healthwatch and the Care Quality Commission, addresses health inequalities across England.
News

Visit your local pharmacy first for seven minor conditions
From 31 January, people across Cheshire & Merseyside can pop down to their local pharmacy for help with seven minor conditions which would previously have required a GP appointment.
News

North West families urged to bring their children forward for routine immunisations this World Immunisation Week
Health chiefs are urging parents, guardians and families across the North West to ensure their children are up to date with their routine childhood…
News

NHS Innovation Accelerator Patient and Public Voices Partners needed.
NHS Innovation Accelerator (NIA) are looking for two Patient and Public Voices Partners (PPVPs) to join the NIA governance groups, to help ensure,…
News

Spring 2024 Covid booster
People aged 75 years and older, residents in care homes for older people, and those aged 6 months and over with a weakened immune system will be…
News
Latest reports and publication
Halton View Care Home - January 2024
Report on our visit to Halton View Care Home on 17 January 2024.
Find out more

Runcorn Urgent Treatment Centre
Patient Feedback report on Runcorn Urgent Treatment Centre.
We carried out five visits to the Runcorn UTC between 30 October 2023 and 23 November 2023.
Each visit lasted between two and three hours and in total 113 people took the time to give us their experience.
We carried out five visits to the Runcorn UTC between 30 October 2023 and 23 November 2023.
Each visit lasted between two and three hours and in total 113 people took the time to give us their experience.
Find out more
Sign up to our news alerts
Stay up to date with what people are telling us about health and social care, our advice and information, and latest reports.