Group A Strep advice
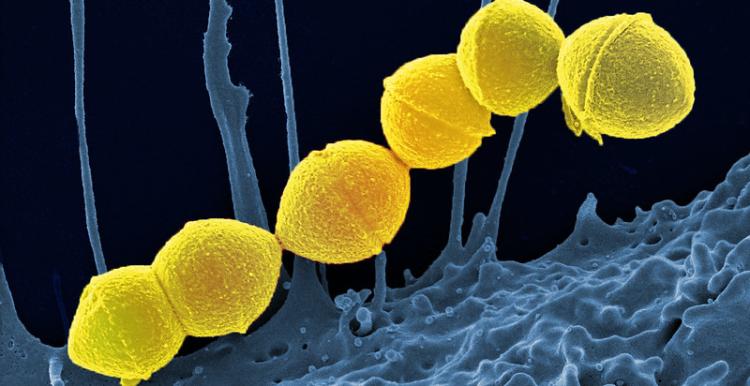
Group A streptococcus is a common bacteria. Lots of us carry it in our throats and on our skin and it doesn’t always result in illness. However, GAS does cause a number of infections, some mild and some more serious.
The most serious infections linked to GAS come from Invasive Group A Strep, known as iGAS.
These infections are caused by the bacteria getting into parts of the body where it is not normally found, such as the lungs or bloodstream. In rare cases an iGAS infection can be fatal.
How is it spread?
GAS is spread by close contact with an infected person and can be passed on through coughs and sneezes or from a wound.
Some people can have the bacteria present in their body without feeling unwell or showing any symptoms of infections and while they can pass it on, the risk of spread is much greater when a person is unwell.
Which infections does GAS cause?
GAS causes infections in the skin, soft tissue and respiratory tract. It’s responsible for infections such as tonsillitis, pharyngitis, scarlet fever, impetigo and cellulitis among others.
While infections like these can be unpleasant, they rarely become serious. When treated with antibiotics, an unwell person with a mild illness like tonsilitis stops being contagious around 24 hours after starting their medication.
What should parents look out for?
It’s always concerning when a child is unwell. GAS infections cause various symptoms such as sore throat, fever, chills and muscle aches.
As a parent, if you feel that your child seems seriously unwell, or is becoming more unwell even if they are on treatment or have recently finished antibiotics, you should trust your own judgement.
Contact NHS 111 or your GP if your child is getting worse despite paracetamol or ibuprofen if:
- the temperature has lasted more than 5 days
- your child is feeding or eating much less than normal, especially if they are drooling or appear in pain when swallowing
- your baby has had a dry nappy for 12 hours or more, or is crying without tears
- or your child shows other signs of dehydration
- feeling thirsty
- dark yellow, strong-smelling pee
- peeing less often than usual
- feeling dizzy or lightheaded
- feeling tired
- a dry mouth, lips and tongue
- sunken eyes (dark circles under eyes)
- your baby is under 3 months and has a temperature of 38°C, or is older than 3 months and has a temperature of 39°C or higher
- your baby feels hotter than usual when you touch their back or chest, or feels sweaty
- your child is drowsy (much more sleepy than normal) or irritable (unable to settle them with cuddles, toys, TV or snacks – especially if they remain drowsy or irritable despite any fever coming down)
Call 999 or go to A&E if:
- your child is having difficulty breathing – you may notice grunting noises or their tummy sucking under their ribs or using their neck muscles to breathe
- there are long pauses (more than 10 seconds) when your child breathes
- your child’s skin, tongue or lips are blue
- your child feels very cold or clammy to touch
- your child is difficult to wake up or keep awake
- your child has severe pains in their arms, legs neck or back
- your child has a painful, red area of skin, especially if it is getting bigger quickly
How can we stop infections from spreading?
Good hand and respiratory hygiene are important for stopping the spread of many bugs. By teaching your child how to wash their hands properly with soap and warm water for 20 seconds, using a tissue to catch coughs and sneezes, and keeping away from others when feeling unwell, they will be able to reduce the risk of picking up, or spreading, infections.


